Lesson 7
Digestive
System and Colic
Digestive System
CHOKE
Obstruction of the esophagus. This is an emergency situation.
Blockage
could be caused by feed, treats, lack of water (especially in the winter) allowing
for feed blockages, chunks of apples or a corn cobs, very coarse hay.
Clinical signs: Coughing, gagging, discharge
of saliva or feed from nose and mouth, dysphagia (difficulty swallowing) and ptyalism (excessive salivating).
The
horse will have difficulty breathing. But unlike humans will still be able to
breathe.
Anxiety, trying to “retch” and
stretching/arching of the neck.
*
Care must be taken when examining the horse as a drooling horse may have
rabies, which is transferrable to humans.
What to do: Call a veterinarian. Do not
delay in calling the veterinarian, as permanent damage to the esophagus may
result. Walk the anxious horse, or let
him stand quietly, and allow the horse to lower his head. Remove feed. Follow
veterinarian’s advice regarding access to water.
Do
not use a water hose to try to dislodge the obstruction. Carefully clean out horse’s mouth if
possible. Massage the left side of neck
over the obstruction (lump). Try to keep
the horse calm.
What the veterinarian will do: Tranquilize the horse. Pass a stomach tube in an effort to gently
dislodge the obstruction. The
veterinarian may give medication to help the esophagus muscles to function more
efficiently and give the horse time to get the obstruction through. Antibiotics
and anti-inflammatory agents are usually indicated.
If
the horses does not improve lavage of the esophagus will be the next step. This requires sedation and the insertion of a
nasogastric tube through which water will be flushed to try to loosen the
blockage. The horse’s head must be kept
low to prevent water from getting into the lungs.
All
horses should be fed a soaked complete feed for 7-14 day, decreasing the chance
of a second choking episode. Horses with
damage to the lining of the esophagus will need to be kept on the soaked
complete feed diet for at least 60 days.
Horses that have repeat issues of choking may have to remain on the
soaked complete feed diet for the rest of their lives. There are surgical procedures that may help.
EQUINE GASTRIC
ULCER SYNDROME (EGUS)
Foals
as well as adults can be prone to developing stomach and intestinal
ulcers. Newborn foals may develop
perforating peptic ulcers because the mucosa is not fully developed. By the time they are a few weeks old the
ulcers should be healed unless stress and poor management has been a part of
the foal’s life, in which case medical intervention is required. Most foals
will not exhibit symptoms of ulcers.
Stress
plays a major role in the cause for all ages of horses. Performance horses are at greater risk due to
stress of training and performance.
Performance
horses with high grain – low forage diet are very susceptible to ulcers. The chewing of forage produces salvia, which
acts as a buffer – protecting the delicate lining of the stomach. Horses on pasture or having access to a
constant source of forage rarely get ulcers.
Studies have also shown
exercise can cause ulcers, especially if the stomach is empty. A common practice among racehorse trainers is
to not feed a racehorse for 24 hours prior to a race. During strenuous exercise the stomach
contracts, pushing the contents up into the esophageal region where there is no
protection from the acid. Tests have
shown the presence of food in the stomach will prevent the acid from being
forced into the upper unprotected area. Withholding forage will cause more
problems than the goal of achieving better performance.
NSAID’s
(Bute or banamine) can also
be a cause.
Ulcers
can also be caused by another illness, due to secondary stress. Stall
confinement and a change in routine.
Clinical signs: adult horses: colic, lack of
appetite, poor body condition score, irritability, poor performance, dull
appearance
In
foals: Most foals will not show symptoms, but be alert for: no interest in
nursing, diarrhea, ptyalism (excessive salivating),
laying on the back with stomach exposed (dorsal recumbency)
and bruxism (grinding of teeth).
Diagnosis: The only way to definitely
diagnose an ulcer is with an endoscope.
Treatment and control: Change of management is the
first step. Treatment with drugs will
not be effective if the cause is not eradicated. Horses that must be kept in stalls should be
offered free choice hay. Grazing and
pasture turnout is the best way to help prevent the formation of ulcers. New studies show some alfalfa hay in the diet
may help prevent the development of ulcers, due to the calcium content acting
like a buffer against the acid.
Drugs: The objective of drugs
is to lower the acid and/or protect the sensitive lining by creating a coating
agent.
Ranitidine,
cimetidine, famotidine – Histamines (H-2 blockers) competes with the histamine
that stimulates the cells to produce acid. Used to treat gastro-duodenal
ulcers. Effectiveness is questioned, best results when horses are removed from
training/competition and the stressful environment. Not approved by the FDA,
but used off-label.
Omeprazole
– proton pump inhibitor; inhibits and shuts down the
production of acid. Approved
by the FDA. Horses can remain in
training. Most effective treatment, but more expensive.
Treats and prevents.
Antacids
- works to neutralize the stomach acid already present. Not proven to heal or
prevent ulcers. High and frequent dosages are recommended.
COLIC

Strangulating vs.
non-strangulating colic.
Conditions
of the small intestine that cause acute colic may be classified as simple
non-strangulating obstructions and strangulating obstructions.
Simple
obstructions occur when intestine is blocked, without concurrent vascular
compromise. A simple obstruction allows the buildup of intestinal contents. The
intestine becomes distended due to the material being blocked from advancing.
Minimal tissue damage is the result, unless the obstruction is allowed to remain
and becomes worse. Examples of a simple obstruction may be ascarids,
feed, or foreign bodies; and obstruction by cancerous growths, abscesses or
adhesions. If the mass cannot be moved
by the use of fluids and mineral oil, surgery will be required. Speed in
treating the horse is imperative.
Strangulating
obstructions can occur when a simple obstruction is not removed. The blood and oxygen supply is cut off
resulting in the severe damage of the intestine. Bacteria and endotoxins are allowed to invade
the intestine.
Strangulating
colic can also be caused by volvulus (twisting) of the small or large
intestine.
When
the intestines are twisted or displaced surgical correction will usually be the
only way to save the horse. It is usually not possible for the vet to
determine, during the early stages of the colic, whether the horse will require
surgery or not in order to cure the colic. The vet will monitor the horse
closely using various diagnostic aids to determine whether surgery will be
necessary. The costs of colic surgery
can run upwards from $5,000, including pre and post-surgical care. If surgery
is contemplated it is wise to understand your horse’s chances of survival. The
veterinarian should be able to give you an educated guess as to the chances of
the horse surviving the surgery.
Mild
colic signs:
a.
Spasmodic colic – spasms of the intestines causing mild abdominal pain.
b.
Simple gas colic – Gas distention of the intestines causing abdominal pain.
c.
Impaction colic – feed which impacts and causes a temporary lack of movement
along the digestive tract, also causing abdominal pain. This includes sand accumulation from feeding
in areas where soil is sandy. Blockage due to ascarids, or the mass removal of the parasite when
deworming.
Any of the above normally
initiates as mild colic signs, but depending on the amount of gas buildup or
the severity of the spasms, can show up as significantly painful to
horses. Any colic in the horse should be
considered an emergency, because it is much easier to prevent colic from
becoming more severe by treating it appropriately as soon as possible.
Prevention:
1.
Feed at same time everyday.
2.
Examine your feeds closely and never feed spoiled feed or moldy, musty hay.
3.
Keep feed amounts and quality consistent.
Increase feed amounts gradually, and change feed types gradually.
4.
Offer horses clean fresh water continuously.
5.
Good horse management practices.
6.
Regular psyllium in the diet (1 –2 cups per 1,000 lbs daily for 1 week a month)
will prevent sand accumulation in the intestinal tract and prevent sand colic.
7.
Maintain a good deworming program, especially for young horses.
What
to do before the vet comes:
Keeping
the horse up and moving is helpful in easing the pain and preventing the horse
from rolling. If the horse is lying down
and is still, forced walking is not a necessity. Follow the instructions of
your vet.
What
the vet will do:
An initial exam to try and
determine the nature of the colic.
Usually pain relievers, antispasmotics, and possibly
mild sedatives may be used to control the pain.
The vet will most likely pass a stomach tube in an attempt to relieve
any gas accumulated in the stomach, or possibly even siphon accumulated fluids
off the stomach. If an impaction is
suspected, mineral oil or other lubricants may be administered into the stomach
via the stomach tube. Rectal palpation
may be performed to aid in diagnosis.

Other
Specific Types of Colic
Blister Beetles
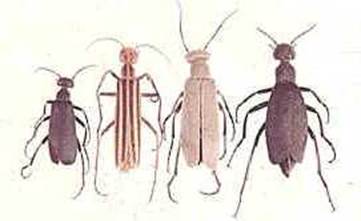
Blister
beetles are found in alfalfa hay occasionally.
They are very toxic to the horse and cause a deadly colic when ingested.
These blister beetles are trapped in the hay during the baling process.
Enteroliths
Hard concretions that can form
in the intestine and cause blockage of the intestinal tract.

Enteroliths have been linked to pastures
or water that is high in calcium or phosphorous (high alkaline sources of water
or feed). These stones can also occur from the horse ingesting a piece of
string or nylon as may be found in halters, lead ropes, hay bags, and even old
tires used as feed tubs.
Prevention
in high alkaline areas of the country consists of adding vinegar (acidic) to
the diet (4 oz per day).
DIARRHEA
Although
horses will develop a loose stool on certain occasions, when a horse has a
persistent or a foul smelling watery diarrhea, you should consider it a
definite emergency.
Colitis
- Inflammation of the colon (large intestine) which can be caused by bacteria
(like salmonella), Potomac Horse Fever, stress, disruption of the balanced
microbial population in the digestive tract, parasites or other causes.
Vital
signs should be taken and communicated to the vet during the initial call.
The
vet will examine the patient, probably take blood and other laboratory samples,
and may initiate treatment with re-hydrating fluids as well as other
therapies. Treatment must be implemented
as laminitis is possible.
Keeping
the horse hydrated is one of the most critical parts of the treatment in cases
of colitis, because the horse can dehydrate so rapidly when they develop
diarrhea.
Prevention: In areas where Potomac horse fever is a
factor, vaccination is wise. Regarding other forms of infectious diarrhea, the
horseman must keep in mind that over work or other forms of physical stress
(physically overstressing the horse’s system) can lower the horse’s natural
immunity and can lead to changes in the colon which could lead to colitis. Avoid the over use of certain antibiotics or
anti-inflammatories (bute or
banamine). Make all feed changes gradually, this
includes forage. Provide clean water.
Internal and
External Parasitic Diseases
and
Their
Prevention and Treatment

Equine Internal Parasites
|
Parasite |
Site of Infection |
Life Cycle |
Symptoms |
Treatment |
Control |
|
Habronema (Stomach
worm) |
Stomach |
Typical, but fly involved |
Typical & wound contamination |
Ivermectins, moxidectin , Strongid, or benzimidazoles |
Good Mgmt., Fly control |
|
Ascarids (large
roundworms) |
Small Intestine |
Typical & larvae migrate through
lung & liver |
Typical & Young horses – cough,
snotty nose, impaction |
Same as above |
Good Mgmt. |
|
Small Strongyles |
Large Intestine |
Typical & cysts in mucosa |
Typical & Colics
in spring when cysts mature |
Same as above moxidectin
and Ivermectins effetive
against cysts |
Good Mgmt. |
|
Large Strongyles
(Bloodworms) |
Large intestine |
Typical & larve
migrate through intestinal blood vessels |
Typical & anemia and thromboembolic
colic |
Same as above moxidectin and Ivermectins effective against migrating larvae |
Good Mgmt. |
|
Threadworms |
Large intestine |
Typical & mares milk to foal |
Foal diarrhea (7 days to 3 weeks of
age)` |
Ivermectins, moxidectin, strongid, benzimadazols |
Good Mgmt&
Prevention- Ivermectins or quest to
mare day of foaling |
|
Pinworms |
Large Intestine |
Typical & eggs sticky found on
rectum and anus |
Typical & tail itching and
rubbing |
Ivermectins, moxidectin, strongid, benzimidazoles (can give when see tail rubbing) |
Good Mgmt. |
|
Bots |
Stomach |
Part of life cycle of Bot Fly
(larval stage in stomach) |
Typical & see bots in manure,
Seasonal – Bot eggs (nits) on chest and upper leg hair |
Ivermectins, moxidectin, in the late fall or early winter |
Fly control. Razor off nits. Warm
water to nits |
|
Tapeworm |
Sml. Int. |
Typ.&mite |
Colic |
Praziquantel, pyrantel pamoate (cestocidal dose – double nematode dose), late fall or
winter |
Good Mgmt |

Bots
Typical
Life Cycle
– Adults in intestines pass eggs into manure; eggs hatch and become infective
larvae, ingested by horse and become egg laying adults in intestines.
Typical
Symptoms
of severe infestation- poor hair coat, pot belly, poor doer, unthrifty, poor
appetite, no energy, anemia, pale mucous membranes.
Good
management practices
1.
Well
fed horses have fewer parasite problems.
2.
Clean
up manure: A. from stalls daily B. from
paddocks every other day C. from
pastures regularly (if possible).
3.
Pasture
rotation.
4.
Good
deworming program (deworm all horses on premises at same time).
5.
Strongid C (daily dewormer)
6.
Don’t
feed off the ground.
7.
Conduct
regular fecal egg counts
8.
Manure
management:
A.
compost pile (heat
kills worm eggs)
B.
Haul off manure
C.
manure spreader – exposes eggs to sun (hot and dry) which kills eggs during
certain season
D.
horses won’t graze where they have droppings.
FECAL EGG COUNT (FEC)
Due
to internal parasites developing resistance to strongyle
and/or ascarid deworming products it is not
recommended to deworm horses that do not carry a worm burden.
Horse owners or stable managers should collect a small amount of manure, secure it in an airtight container. The sample must not be allowed to freeze, but
should be refrigerated and sent to the lab within 12 hours of collection. At
the lab, a technician mixes the manure with solution. The worm eggs float
to the top. A gram of the specimen is examined under a strong microscope
and the eggs per gram are counted.
Most labs just count small strongyles.
Large stronglyles, in all stages, are easily
controlled. If the small strongyle population
is controlled then so goes the large. If a horse has a high population of
small strongyles, he generally also has ascarids.
Using the FEC to detect tapeworms is not reliable. Tapeworms infrequently
shed segments which may contain eggs (needed for detection). In
comparison, other intestinal worms shed eggs almost continuously.
The lab will report the small strongyle egg
count as eggs per gram. The FEC scale is: less than 200 eggs per gram -
low; 200-500 eggs per gram - medium; 500 plus - high.
Horses with a FEC of 200 or more are candidates for colic, unthriftiness
and anemia. These horses are also contaminating the pasture and keeping
the parasite growth cycle active.
Conducting a second fecal egg count 14 days after a dewormer
has been administered will tell you if the product worked. A low fecal
egg count reduction (FECR) can indicate parasite resistance to the active ingredients
in the product. A low count may also indicate the product was old or not
enough administered. The horse should be dewormed with a product that
uses a different chemical class as the active ingredient. Then another
FEC conducted within 10 - 14 days.
Horses with a steady fecal egg count of less than 200 eggs per gram may only
need to be dewormed twice a year. Deworming horses that do not need to be
aggressively dewormed is expensive and can create resistance to dewormer ingredients.
Many vet clinics will do a fecal test to detect worms, but not count the eggs
per gram. In order for the test to be beneficial you must request a
count.
Horses
will still need to be dewormed for bots, pinworms and tapeworms, if so
indicated.
For a more in-depth study of fecal egg counts and the American
Association of Equine Practitioners Parasite Control Guidelines, please go to: http://www.aaep.org/custdocs/ParasiteControlGuidelinesFinal.pdf
DEWORMING PROGRAM
Readily Available Dewormers:
Ivermectins: Eqvalen, Zimecterin, & Quest
- These will get all worms and bots.
Benzimidazols: Anthelcide, Panacur - These will get everything, but the bots
Pyrantel: Strongid, Strongid C – These products will get everything, but
bots. They are also available as a daily
feed additive for constant control of parasites (except bots).
Praziquantel:
This is a recently available compound that controls tapeworms. It is found as an addition to Ivermectin wormers (Zimecterin Gold),
Quest (Quest Plus) and other
combinations, as well as by itself in some products.
Deworming
Schedules – If not conducting fecal egg counts
Foals – Every 2 months until 1 year of age then
deworm as an adult horse.
Adult Horse – Every 3 months - fall (after first
frost) and spring. Deworm for bots and all roundworms. (Quest or ivermectins)
Summer and winter – deworm for
all roundworms. (Strongid,
pyrantel, benzimidozoles)
Daily worming - Strongid
C - Still must worm for bots fall and spring.
Care must be taken when worming
a heavily infected young horse. Large roundworms may cause impaction colic.