Health and Disease Management
Lesson Four
Hind Limb Lameness
Hip Disorders
Although hip
disorders are not common in the horse, if a horse is lame due to a problem in
the hip, it is usually associated with osteochondritis dissecans (OCD) in the
hip joint, or an injury from a trailer accident or something similar. These
injuries are usually very difficult to correct and may cause permanent
lameness. The following is an outline
of some of the more common hip and thigh disorders.
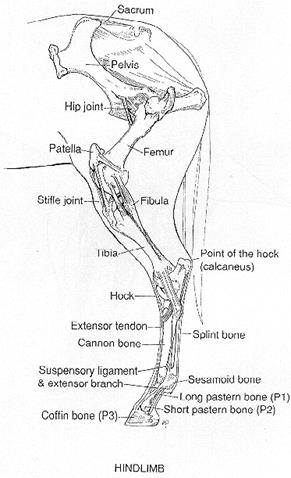
A. Pelvis
B. Femur
C. Patella
(knee cap)
D. Stifle Joint
E. Tibia
F. Hock Joint
I. Fractures of the Pelvis
A. Knocked-down Hip (one hip will be
lower when the horse is standing square)
1. Refers to
fracture of the point of the hip which causes that point to be knocked down)
2. These horses
can be sound for some things after stall confinement healing from 3 to 6
months)
3. Identified
by the lack of a point of the hip on one side compared to the other side.
B. Fractures
within the acetabulum (fractures in the socket part of the joint are very
serious and will result in an unsound horse for life)
II. Fractures
of the Femur
A. Complete fractures are devastating
in the adult horse and usually require euthanasia.
III. Other Hip
and Thigh Injuries
A. Rupture of the round ligament of
the femur
1. Toe and
stifle turn out.
2. If there is
coxofemoral joint luxation, one leg is shorter than
the other.
3. In either
of these conditions future soundness is unlikely.
B. Trochanteric bursitis
1. Whorlbone lameness. Soreness
over the trochanteric bursa located at the top of the femur. * A bursa is a space that is filled with
fluid in areas where friction may develop.
Usually causes
a horse to travel like a dog would move. Inside quarter of shoe wears more than
outside quarter due to the way the horse brings the foot down.
2. Seen most
often in Standardbred trotters and pacers.
C. Fibrotic and ossifying myopathy
1. Fibrosis
and calcification of the semitendinosis and semimembranosis muscles (muscles in buttocks area below the
point of the buttocks)
2. Seen in
performance horses (reining and rodeo horses) that make sliding stops can be
prone to this lameness.
3. Butt bars
on trailers can cause this injury during hauling.
4.
Characteristic gait seen at a trot. Horse
will jerk the limb back noticeably before the foot hits the ground. If the lameness is severe enough to cause a
problem, a surgical removal of the hardened and calcified area of muscle is
performed. If the horse is able to
perform adequately with the muscle scaring and calcification, physical therapy
procedures will partially relieve the restriction of movement and reduce the
pain.
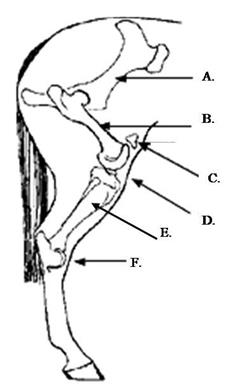
Stifle Disorders

The Equine Stifle Joint
A.
Location of the Stifle Joint
The
stifle area is often injured in the horse, but luckily, because it is similar
in anatomy to our own knee, we have lots of experience and can correct
problems. Problems that can be associated
with the stifle are:
I. Upward fixation of the patella (locked up in
the stifle).
This is usually seen in the horse with
the straight up and down conformation behind. (post
legged behind). The patella (knee cap) locks in position on occasion to prevent
the horse form being able to flex his stifle or hock temporarily.
To see a horse do this is quite
startling, the horse will drag the hind leg affected with the stifle and hock
unable to bend and the toe of the hoof dragging the ground. The affected hind
leg will extend behind the horse. This can happen quite suddenly, usually when
at a walk, and can pop back into normal position just as fast.
If you are unable to get the horse to
pop back into normal position, back him up a few
steps, or massage the affected stifle and it will usually pop back into normal
position.
For horses that continually have this
problem, a veterinarian has two surgical options: (1). medial patellar desmotomy (MPD) an
operation that clips the stifle (cutting the medial patellar ligament
(MPL)). MPD should be a last resort
treatment (because of future arthritic problems in the stifle caused by this
surgery) it does prevent any further locking up. (2.) ultrasound
guided precutaneous splitting (USGPCS), the medial
patellar ligament is split instead of cut.
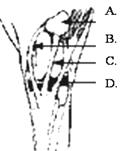
Upward Fixation of the
Patella
Stifle Joint – Front View
A. Patella B. Lateral Patellar Ligament C. Middle Patellar Ligament D. Medial Patellar Ligament
(locked up in the stifle)
A. Upward fixation of the patella (summary)
1. Locked up
in the stifle (Stifled)
2. Predisposed
by post legged (straight up and down) conformation
3. May be seen
more often when a post legged horse has been fatigued in those muscles from
over work or long trailer rides.
4. Backing the
horse will often allow the stifle to pop back into normal position. If this
doesn’t work, massaging around the muscles of the stifle and attempting to
manipulate the joint might be helpful in popping it back to normal.
5. In horses
that continuously lock up, clipping or splitting the MPL may be needed,
followed by physical therapy. These surgeries must be reviewed carefully as
complications can result.
II. OCD of the
stifle
A. Seen in the young horse (yearling
to 2 year old)
B. Difficulty getting up and down due
to stiffness in the stifles, usually both stifles are involved;
joint swelling and lameness are apparent
III. Sprains,
Strains, meniscus and ligament injuries to the stifle
A. Not seen as
often as in human athletes. Horses don’t do the twisting and turning and are
four legged.
B. When this
type of injury occurs in the horse, surgery is not very helpful.
Horse will normally not be sound for future use. Pasture sound is expected once
healing is complete.
Tibia and Hock Disorders
I. Tibial Fractures
A.Very
serious. Can be life threatening.
B. Sling may help
save a horse
C. Hairline tibial fractures seen on some young racehorses.
D. Surgical
repair necessary on serious fractures.
II. Rupture of
the peroneus tertius
A. Caused by
rapid starts (out of starting gate or box)
B. Hock will
stay in extension when stifle flexes.
C. Horse is
not badly lame, just “goes off”
D. 3 to 4
month healing time.
E. Soundness
is expected after healing.
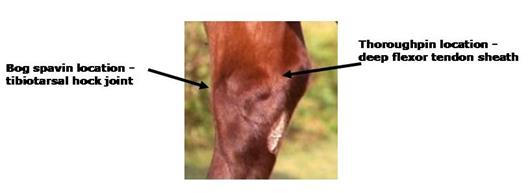
III.
Thoroughpin
A.
Inflammation of deep flexor tendon sheath.
(Refer to hock diagram at the end of the lesson) The
swellings will be soft and fluid-filled, and may appear on both sides of the
hock, slightly higher than where a bog spavin will be located.
B. Lameness is
usually not present.
C. Could be
considered a blemish.
D. Straight
hocks predispose to strain in this area
IV. Slab and
chip fractures within the hock joints.
A. Treated
same way as knee chips and slabs, with arthroscopic surgery.
V. Bone spavin
A. Bone
spavins are the most common cause of hind limb lameness in the horse. It is
osteoarthritis (degenerative joint disease – DJD).
B.
Inflammation of the two lowest joints of the hock (the tarsometatarsal
and the distal intertarsal joints), with the third
joint, the proximal intertarsal, being the least
likely to develop bone spavin. (distal – away from the center of the body – the
outside)
C. Usually
results in calcium buildup in and around these joints.
D. Spavin test
will exaggerate lameness. (Flexion test of the hock joint)
E. Manage pain
and inflammation to continue to use horse. Can be career ending.
F. If joint
fixes in place the pain from the condition will be greatly relieved.
VI. Curb
A.
Inflammation and enlargement of the plantar ligament (runs down the back of the
leg, below the hock) or tendonitis of the flexor tendons.
B.
Sickle and/or cow hocks predispose to this condition.
C. Usually
causes mild lameness.
VII. Bog
Spavin
A.
Inflammation of the tibiotarsal hock joint. (The joint of the hock that moves.)
B. Soft fluid
filled swelling on the inside front of hock, with a smaller swelling on both
sides.
C. Often
associated with OCD of the hock.
D.
Usually causes mild or no lameness.
VIII.
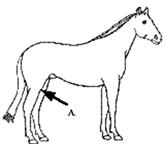
Stringhalt
A. Over
exaggerated upward flexion of the hind leg at a walk, lesser degree at the
trot, and not apparent at the canter.
The hind foot is drawn up suddenly and hits the underbelly, then strikes
the ground on return movement.
B. Cause maybe
unknown probably associated with nerve over-stimulation. One type: Australian
stringhalt is caused by eating a toxin on certain plants, specifically: sheep’s
sorrel, couch grass, flatweed and sweet pea.
C. Treatments
are not normally very successful at correcting the abnormal gait completely.
Parts of the Hock
IX. Capped
Hock
A. Just like a
shoe boil in the elbow, but it’s over the point of the hock.
B. A blow to
the point of the hock or kicking at a trailer gate.
C. Usually
doesn’t cause lameness, but causes blemish.
D. A vet will
normally drain and inject the area.
X. OCD of the
hock
A. Often
associated with bog spavin and has been thought to be a cause of later forming
bone spavin.
B. Can be seen
in all ages of horses.
C. Lameness is
not always present, but joint distention is apparent (swelling)