Lesson 3
Common Hoof
Disorders
Sole Bruises
Definition – Sole bruises
are actual bruising (bleeding) under the sole surface of the horse’s foot.
(Remember – the sole is not intended to be a weight bearing part of the bottom
of the foot, it is normally concave and shouldn’t hit the ground surface with
full force.)
Symptoms – There is some
sensitivity over the bruised area especially if hoof testers or some other
pressure is applied over the bruised area. It doesn’t always cause a noticeable
lameness. Paring away of the sole in the
bruised area will show discolored (bluish-black) sole .
Causes – Concussion to the sole
by hard objects such as large rocks, gravel or hard road surfaces. Unleveled or poorly fitting
horseshoes can also cause sole bruises.
Location – the under part of
the sole surface of the hoof
Prevention – Shoeing the horse
will help protect the sole. Keep the sole of the foot in a healthy
condition. Pads are used when the sole
is flat or not very tough.
Treatment – Treatment would
consist of Epsom salt soaks, toughing up the sole with hoof conditioners
(iodine or koppertox) and the use of pads for
protection of the bruised area, if the horse is to continue to be used.
Corns
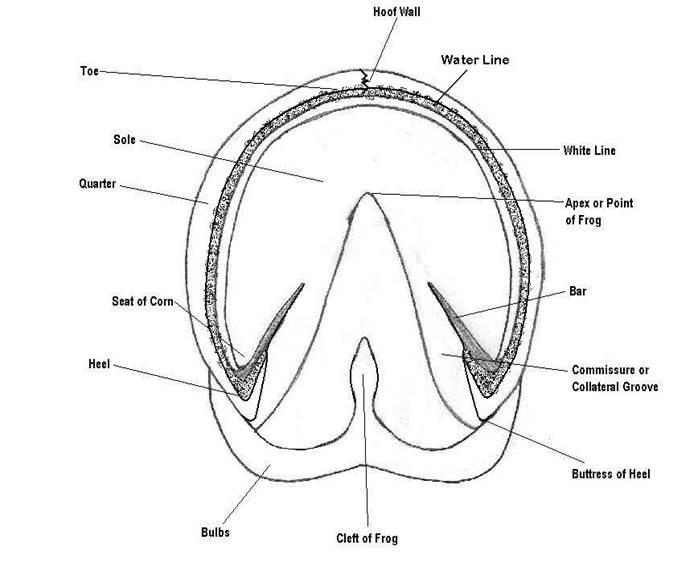
Corns are a sole bruising which
occurs in the “seat of corns,” the area at the heel formed by the angle of the
bars of the heel. See foot chart. The
bruising is usually due to a shoe that has been left on too long. The foot
grows back and the end of the shoe will put pressure on the sole area at the
angle of the bar. When the horse walks or moves on the shoe in this position,
it puts pressure in an area that is not designed to bear weight so it will
easily bruise.
Hoof Abscess
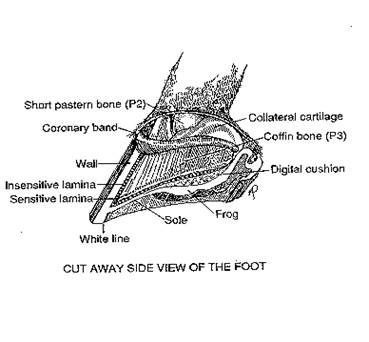
Definition – A hoof abscess in
an infection or pus pocket on the underside of the sole or somewhere within the
sensitive part of the hoof.
Symptoms – A severe lameness,
the horse is normally reluctant to put any weight on the affected foot until
the abscess breaks and drains. There is heat in the affected foot, especially
where the abscess is located, and hoof testers or thumb pressure over the
abscess will illicit a pain response in the horse. Oftentimes there will be
swelling in the pastern area, and a strong digital pulse can easily be felt in
the affected foot.
Causes – A sole bruising, if
severe enough, can develop into a hoof (sole) abscess. The most common cause of
the hoof abscess is a puncture wound of the sole or frog that penetrates into
the sensitive tissue. White line disease or other separations of the hoof area
that allow bacteria to penetrate into the sensitive structures of the hoof can
cause a hoof abscess. Abscesses can also develop in the space that is created
when the coffin bone rotates during a severe case of laminitis. “Quicking” a horse
(driving a nail into the quick, or sensitive part of
the foot) can cause an abscess.
Location – An abscess can occur
anywhere below the hoof capsule in the sensitive part of the foot, but usually
follows the path of least resistance, so many will travel to the white line,
then break out at the coronary band.
Prevention – Keeping the foot
healthy, clean and dry, will help prevent hoof abscesses from developing. If the horse is “quicked,”
or gets a puncture wound, paring it out with a hoof knife, or treating it
immediately with strong iodine may help prevent a hoof abscess from
developing. Putting the horse on preventative antibiotics may also be
warranted. Seek advice from your veterinarian anytime you see blood coming from
a hoof puncture.
Treatment - Hot Epsom salt soaks will help draw
the abscess out of the hoof, as will a poultice application under a hoof
bandage. Both procedures should be
used. Consult your veterinarian if the
abscess does not resolve within a few days.
Antibiotics may be necessary. Once the abscess breaks and drains, you
should still soak and pack for a few days, treating the open area with
something like strong iodine to toughen the area and close the opening.
Hoof Cracks
Definition – a vertical crack in the
hoof wall. Cracks can be superficial (not penetrate the sensitive lamina) or
deep (penetrate the sensitive lamina and cause blood to appear at the surface.)
There are three “named” types
of hoof cracks.
A “sand crack” originates at the coronary band and
continues toward the toe of the horse, running parallel to the horn tubules,
either completely or partially to the edge of the hoof. These cracks can be thought of as a fracture
of the hoof wall.
A “horizontal crack” is parallel with the coronary band and
grows out with the hoof.
A “grass crack” originates toward the toe and runs parallel
to the horn tubules toward the coronary band.
These cracks can be thought of as a “split” in the hoof wall.
Cracks are identified by location, and are called toe,
quarter or heel cracks. On the bottom of
the foot, or solar aspect, cracks usually go across the bar or sole and radiate
from the apex of the frog, and then are called, “bar” or “sole” cracks.
Symptoms – If the crack is
superficial, there are no lameness symptoms, but if the crack penetrates into
the sensitive tissue of the hoof, blood and pain will be noticed.
Cause – Dry, brittle hooves are more
prone to hoof cracks. Cracks can also occur from imbalanced feet or uneven
weight bearing. A deep wire cut or laceration into the conorary
band will produce a defect in the coronary band where the hoof grows from, and
a crack will always grow down from there for the rest of the horse’s life.
Location – the location of the hoof
crack is usually designated by toe, quarter or heel crack. They can start from
the ground surface and travel up, or they can start from the coronary band and
travel downward.
Prevention – Good hoof management
practices will help prevent hoof cracks. Keeping the hooves
healthy and pliable. Proper balancing and shoeing will also prevent hoof
cracks.
Treatment – The important aspect of
treating hoof cracks, is to stop the crack from
spreading, stabilize it the best you can, and promote healthy hoof growth to
allow the crack to grow out as quickly as possible. The crack can be grooved
with a horizontal groove in the hoof wall at the end of the crack. This might
keep it from spreading, especially if it is not a deep crack. Usually a horse-shoer and /or a Veterinarian will be involved in the
treating of a hoof crack. They will use shoeing (shoes with clips to stabilize
the crack, or a shoeing technique to take direct pressure off the crack) . OR they may use staples, or other hardware (screws and
plates) or even special acrylic bonding material to repair the crack. (Remember
horses’ hooves grow down about 1/4 to 1/3 of an inch a month). Trimming or re-shoeing should be done every
four weeks until the crack has been resolved.
Navicular disease or syndrome (CAUDAL HEEL SYNDROME)
Definition – Navicular disease, or as
it is more popularly referred to by veterinarians today, “caudal heel
syndrome”. It is a chronic (long
standing) disease involving inflammation of the navicular bone and navicular
area of the front limbs.
Symptoms – Navicular disease usually
shows as a mild to medium lameness condition of the front limbs, usually one
front being worse than the other. The horse is normally reluctant to place his
heels to the ground at a trot, and will stumble and short stride. A head bob is
usually noticeable at the trot (head goes up when the sorest foot hits the
ground) especially when going in a circle. When standing, a
horse with navicular pain may point (place one front foot slightly ahead of the
other, therefore relieving the pressure on the navicular bone). X-rays
of the navicular bone will show spurring of the bone and /or holes in the
navicular bone (lollypop looking holes). Although occasionally a horse with
clinical navicular disease will have clean x-rays. In this case the explanation
is usually that the pain is associated with the soft tissue structures of the
navicular area. (This is still considered to be navicular disease)
Location – Navicular bone, navicular
bursa, and deep digital flexor area over the navicular bone. Seen almost exclusively in the front feet. Usually both
front feet are involved, one worse than the other.
Cause
- Usually seen in older horses as a wear and tear type of damage, seen in
horses with small hooves, short, straight pasterns, or low heels and long toes.
Concussion over this navicular area below the heel is the main cause. Heredity
may play a role, and horses as young as two-years old can start showing
symptoms.
Prevention – Short, straight pasterns
and small feet can predispose a horse to navicular problems because of the
increased concussion to the heel area and navicular area of the foot over time.
Purchasing horses with adequate size of foot in relation to their size, as well
as those with good pastern conformation, and normal and equal hoof to pastern
axis, as well as keeping these horses shod in the correct way, can prevent you
from having problems with navicular disease in your horses.
Treatment – Corrective Shoeing or
trimming – High heels, short and rolled toes . Bar
shoe, bar across the middle third of the frog.
Medical management: Bute - pain management. Isoxuprine tablets in the feed will help increase blood
flow to the navicular area.
Laminitis
Definition – Inflammation of the
lamina of the feet.
Causes:
1.
Overloading the digestive system with carbohydrates and starches; overfeeding
grain, lush pasture or rich hay are a few examples. This is the most recognized cause of
laminitis.
Horses
diagnosed with Cushing’s syndrome, Equine Polysaccharide Storage Myopathy,
abnormal thyroid levels or are insulin resistant must be offered diets which
avoid carbohydrates and starches.
2.
Obese/overweight condition.
3.
Retained placenta.
4.
High fever, infection from disease.
5.
An allergic reaction to a vaccine or medication.
6.
Exposure to black walnut shavings.
7.
Excessive cold water ingestion when an excessively hot horse is not cooled out
properly.
8.
Road founder – overwork on hard ground.
9.
Overexposure to cortisone type drugs
All
above basically encompass over stressing a horse due to poor training or
management decisions. (Pushing a horse over what his system can tolerate) Horse
must become slowly accustomed to changes in things like feed, or exercise)
Three Phases of Laminitis:
DEVELOPMENTAL
PHASE – This
is the period when something occurs to the horse or pony leading to the
inflammation of the laminae. It is sometimes
very difficult to recognize a horse in the developmental stage of
laminitis. Observation and awareness is
the key – know if your horse has had access to the feed room, excessive amounts
of lush grass, has been vaccinated recently, has had a high fever, or any of
the other causes listed above.
There
are some cases where the cause is never determined.
It
is recommended as part of the daily routine to check the horse’s digital pulse
and hoof temperature. If either is
elevated now is the time to apply ice and start preventative treatment.
If
treated during this phase you may be able to prevent the laminitis. Treat with NSAID’s, lower blood pressure, and
laxatives if overeating of grain is suspected.
Research
has shown applying ice to the hooves during the developmental stage of
laminitis may prevent the onset of the acute stage. Dr. Chris Pollitt, researcher for the
University of Queensland, Australia, recommends the horse stand in ice 20
minutes twice a day with the time being extended to one to two hours depending
on the severity of the condition. During
research horses have stood in ice for 2 days straight with no detrimental
effects. (Click here for more information on
laminitis research.)
The
developmental stage may last 12 – 50 hours depending on the cause.
ACUTE: After the developmental stage the horse may
enter the acute stage. This is when the
first signs of hoof pain occur and many people first realize something is
wrong. Elevated hoof temperature and
bounding digital pulse may be apparent.
The coronary band may be swollen and distended. The horse may stand in the classical
laminitis stance of front legs extended trying to relieve pressure on the toes.
X-rays
of the hoof should be taken at this point. They will serve as a baseline for
future x-rays, show if the coffin bone has rotated from a previous laminitis
episode and allow a measurement be taken of the distance between the dorsal
hoof wall and the dorsal cortex of the distal phalanx. If the coffin bone shows severe rotation at
this early stage of laminitis the prognosis is poor.
Treatment
during the acute stage of laminitis is aimed at alleviating pain and minimizing
further damage to the hoof.
The
use of anti-inflammatory drugs (NSAID’s) to make the horse more comfortable is
usually recommended. Phenylbutazone
(bute) appears to be the
most effective drug. Care must be taken
the horse is not made too comfortable and moves around excessively – causing
more damage to the hoof. The dose used
should take the edge off the pain and give him some relief.
The
attending veterinarian may recommend a vasodilator agent, but research has not
proven these drugs effective treatments in laminitis.
Most
veterinarians will recommend the horse be confined to a stall and the shoes be
pulled. These steps will lessen further
trauma to the already weakened laminae.
The
common mechanical treatment of the hoof is aimed at aiding break-over,
elevating the heel in order to decrease the force on the deep digital flexor
tendon and supporting the palmar/plantar (digital cushion) part of the
foot.
Dr.
Stephen O’Grady, farrier and veterinarian from the Northern Virginia Equine
Facility (http://www.equipodiatry.com),
recommends the following treatments be implemented.
To
remove the stresses placed on the laminae at break-over, a line is drawn across
the solar surface of the foot approximately ¾ inch dorsal to the apex of the
frog. The hoof wall and sole are beveled at a 90 degree angle dorsal to this
line using a rasp. This effectively
decreases the bending force or lever arm exerted on the dorsal laminae. It also
moves the break-over point back. Heel
elevation and support can be applied in one of three ways.
1. Sand is a readily available, inexpensive and
often-effective
form of foot support. It provides even support over the
entire
solar surface of the foot, and it allows the animal to angle
its
toes down into the sand, thus raising the heels and changing
the angle of the fetlock.
2. The use of 3-inch high-density industrial
Styrofoam has gained
popularity as a form of foot support. When applied to the
foot,
the weight of the horse crushes the Styrofoam, forming a
resilient mold in the bottom of the foot. It is easy to
apply, is
very forgiving, and it provides heel elevation and good
ground
support. Additional heel elevation can easily be fabricated.
Once the horse has crushed the
original piece of Styrofoam,
this piece is cut in half and the palmar half is retained
and
used as a heel insert. Another full sized piece of Styrofoam
is
applied underneath it.
3. The third method
utilizes a commercially available combination
of
two 5-degree wedge pads that are riveted together, along with
an
attached cuff so they can be taped to the foot.
These wedges
are combined with a resilient silastic material
placed
in the bottom of the foot for support.
This method is
used
on horses that have underrun heels, a broken hoof
-pastern axis or
radiographically show a negative heel angle
(the
solar margin of P3 is lower at the heels than at the toe on
the
lateral radiograph). To apply this
method, fill the bottom of
the
foot with dental impression material, hold the foot up until
the
impression material sets, place the foot in the wedges and
tape
in place. This method provides the best
heel elevation. All
of
the above support methods are easy to apply, provide firm,
but
forgiving support and allow easy removal to examine the
bottom
of the foot. They also provide uniform
support to the
frog,
sole and bars in the palmar/plantar two-thirds of the foot.
This is
accomplished without causing local ischemia and
pressure
necrosis which may occur if treatment is reliant on
frog
support alone.
The acute stage lasts until
the horse recovers or enters the chronic stage of laminitis.
CHRONIC: Not all horses will enter the chronic stage
of laminitis. Research has shown only 15
to 20 percent of the horses in the acute stage will progress to the chronic
stage – if proper treatment was implemented at the developmental and acute
stages.
The
chronic stage is when the laminae have died allowing the distal phalanx (also
known as the coffin bone, pedal bone or P3) to drop or rotate downwards. The signs usually exhibited by the horse are
persistent lameness, mechanical collapse of the foot, abscesses, and deformity
of the hoof wall. The horse is now
foundered (the coffin bone is sinking.)
The
treatment goal is to realign the displaced coffin bone; a goal usually
unattainable. Corrective trimming and
shoeing are the common methods used. Dr.
O’Grady has had much success with the use of glue-on shoes. (http://www.equipodiatry.com/chronlam.htm) More radical surgical treatments, such as
accessory ligament desmotomy or deep digital flexor tenotomy may be attempted.
Each case is different with different results, so the treatment of
choice may vary.
The chronic stage can last
indefinitely.
